From March 19 to April 21, Puerto Rico’s Bureau of Forensic Science had taken 41 samples from corpses.
(Photo by Dennis M. Rivera Pichardo | Centro de Periodismo Investigativo)
By Omaya Sosa and Jeniffer Wiscovitch
Versión en español aquí.
SAN JUAN, Puerto Rico — One of the most important factors to confirm the real status of the COVID-19 case fatality rate in Puerto Rico is conducting molecular tests on people who die and who had any symptoms of the disease.
However, hospitals —which is where most people on the island die— have not been testing all suspected patients and none of the deceased, Puerto Rico’s Secretary of Health Lorenzo González Feliciano admitted on Tuesday to questions from the Centro de Periodismo Investigativo (Center for Investigative Journalism, CPI for its acronym in Spanish). More than 60% of deaths in Puerto Rico occur in hospitals, according to Demographic Registry data.
The official answered the question during a press conference on Tuesday about the status of COVID-19 on the island, when he also reported that disease-related deaths were already at 64 and that, of those, 19 were detected through the annotations that doctors make on death certificates they send to the Demographic Registry of Puerto Rico. González said some of those cases lack confirmatory tests, but did not specify how many of them, and answered categorically that the hospitals have not been taking the samples. By Wednesday the death toll had risen to 67, and the agency’s data dashboard claims that 46 of them come from positive tests and 21 come from medical reports submitted to the Registry.
“Part of the COVID death claims come through the Demographic Registry. Not everyone who is within the Demographic Registry’s frame of reference tested positive for COVID,” he said.
González added that “the only thing that the US Centers for Disease Control and Prevention requires is that there be a certification from the doctor establishing a relationship between COVID and the death [to consider it] as COVID-positive.”
Aren’t hospitals testing the deceased?, CPI asked.
“No, not at this time,” the Secretary responded. When asked why hospitals are not complying with a directive from the Health Department, he said, “basically there was no protocol in place of any kind” and that he is currently in talks with hospitals to see how confirmatory samples can be taken from the deceased prospectively.
This despite the fact that on March 20, the Health Department issued a protocol, signed by former Interim Health Secretary, Dr. Concepción Quiñones de Longo, that orders hospitals to take nasopharyngeal and oropharyngeal samples from all suspected COVID-19 patients who die on their premises. According to the document, said samples were to be sent to the Health Department Laboratory for processing.
Puerto Rico’s Hospitals Association President Jaime Plá insisted that hospitals do know how to handle the issue of deaths but alleged that he does not remember having seen the Health Department’s protocol for COVID-19 testing of the deceased. He argued that if a doctor certifies that the death was a COVID-19 case based on his or her clinical judgment, there is no need to do the test.
“The suspicion process ends by certifying a cause of death,” Plá alleged.
The executive added that in very few cases doctors leave the cause of death entry empty and that he “assumes” that in those cases they would have to do the post mortem test, but he could not confirm if they are doing it.
“If there’s a case where the doctor leaves the death certificate empty, I imagine they have to perform it [the test]. But if the doctor certifies what happened, there’s no specific reason to run a test,” Plá said.
On the other hand, taking samples from suspected patients who die at home is Puerto Rico’s Bureau of Forensic Science’s (NCF, in Spanish) responsibility, and the agency has been taking and reporting them on a daily basis, Commissioner María Conte said in an interview with the CPI.
From March 19 to Tuesday April 21, the agency had taken 41 samples from cadavers, of which four yielded positive, 31 negatives, and six were waiting to be processed by the Health Department Laboratory, which is delivering the results in 24 to 48 hours.
The official confirmed that the NCF has already released the purchase order for the materials needed to adapt its DNA laboratory and begin processing the tests in-house, which should happen in the next three to four weeks.


Dr. Maía Conte (Photo by Dennis M. Rivera Pichardo | Centro de Periodismo Investigativo)
Still, the NCF faces the roadblock of molecular test reliability when more than two hours pass between the time of death and the sample collection. The NCF has had cases where two to three days have passed before the body can be sampled.
Although she acknowledged that the time elapsed in these cases can affect the reliability of the result, Conte said they have taken the samples anyway and some of them have tested positive.
“Theory is one thing and practice is another,” she said.
She also said she has managed to validate the reliability of the results they are obtaining so far, by monitoring the relatives of suspected cases that came up negative. So far, the agency has not detected any family member who develops the symptoms.
Conte confirmed that the NCF runs a second checkpoint to ensure that COVID-19 deaths are properly accounted for and is the evaluation done on all cases of deceased who request a cremation permit.
Even if the body has not reached the NCF, NCF pathologists evaluate the cremation permit form and the death certificate in these cases. As opposed to what happened in Puerto Rico after Hurricane María, when most of the victims were not properly categorized in death certificates and the death toll was significantly underestimated, so far the trend they are seeing is that doctors are making the corresponding entry for COVID-19.
Also, unlike the Hurricane María emergency in 2017, when the NCF was unable to manage the overload of bodies and autopsies, this time the agency has experienced a significant drop in cases, due to the effect that the early lockdown has had on the drop in violent crimes and accidents, the two main categories of cases that this investigative agency usually handles, Dr. Conte said.
In spite of this, the number of corpses that are ready but waiting to be collected in recent weeks has more than doubled: they are usually around 20 and right now there are between 40 and 50. The situation responds to a combination of factors caused by the COVID-19 emergency in Puerto Rico, among which the fear of contagion of funeral agents to handle the bodies and the increase in the work volume at the crematoriums, since burials have decreased, stand out.
The pathologist said that when talking with funeral home directors, they could not identify a single common cause for the lag, but rather the combination of a number of factors.
The CPI interviewed funeral home directors and confirmed the fear of contagion that exists among industry workers and the spike in cremations, mainly associated with a change of mind by relatives of the deceased due to the complexities caused by the pandemic. The CPI has not been able to obtain data to determine if the trend implies that there is a net increase in deaths on the island, or if it is only a transfer of the volume from burials to cremations.
Emmanuel Rodríguez, president of Celestium The Crematory in Carolina —Puerto Rico’s main cremation center— told the CPI that the case volume has doubled since the COVID-19 emergency started and they had to add two cremation machines, which they usually have on backup, to the two they regularly use. The last time they had to activate these machines was after Hurricane María, he said.
When examining the death certificates, both he and other funeral homes have noted “quite a few” cases with respiratory problems, Rodríguez added.
Robert Molina, general manager of the Ehret Funeral Home in San Juan, agreed on the trend of increased cremations and added that 52% of the cases they handled in March were cremations. Although burials are still possible, gathering people at funeral homes is prohibited and there are people who prefer to keep the urn with the ashes to have a ceremony when the emergency is over, he said.
Regarding the fear of contagion, Rodríguez said they handle all cases as if they were positive, they do all the paperwork online and by phone, and they accept just one person to organize the service, either under a tent or from the car. However, there are funeral homes that don’t want to pick up cadavers and independent carriers are charging as much as $1,000, when they usually charge between $80 and $100, due to the risk they believe is associated with transporting the body.
Hilton Lugo, president of the Federation of Carriers and Funeral Directors, confirmed to the CPI that some independent carriers or funeral directors have increased their rates. He said he is charging $500 to transport those who died from COVID-19 on his routes out of Ponce and Mayagüez. If they have to deliver a body to San Juan, he charges $800.
“It’s not about the money, it’s because it’s very risky for us,” said Lugo.
Molina said that although funeral homes are used to dealing with infectious diseases, COVID-19 is something new and the extent of the risk is still unknown.
Dr. Conte said the risk of contagion with COVID-19 is greater when coming into contact with a living person than with a deceased person, provided that they strictly adhere to the cadaver management protocol, since the virus is transmitted by droplets and secretions expulsed by the living that the dead do not produce.
She said they have educated funeral agents and their staff on the protective equipment they should wear as well as the special bags they should use for the bodies. The policy is to treat all cases as if they were positive and, in addition, the NCF labels body bags accordingly with a “positive” or “suspect pending evidence,” status.
Molina said there is fear among funeral home directors because, even though the risk of infection with a deceased is lower than with the living, it’s not “zero” because there is always the possibility that the body will expel gases and tissue.
Meanwhile, both funeral home executives expressed dissatisfaction with the lack of information regarding the COVID status of the deceased. They said suspicious cases and final test results are not always notified on a timely basis.
Rodríguez said they are not being informed if the person is positive or suspicious of the virus, and they end up finding out through family members or because the death certificate lists “Suspected COVID” as the cause of death.
By law, cremations have to be held 48 hours after the time of death, but in positive or suspicious cases, the government has authorized them to be cremated sooner. However, crematories are having to wait 48 hours due to the lack of communication.
“If I’m not told that it came out positive, I can’t do the cremation,” he said.
Funeral homes are concerned “because the information, usually from Forensics and Health, says that we should treat all cases as if they were positive, but they’re granting a waiver to cremate the body immediately if it’s positive. How are we going to know if we can cremate it immediately, if they don’t tell us that it didn’t come up positive? They have to inform us, we find out about it from the family.”
Likewise, Molina mentioned the case of a person who died in a hospital emergency room and was transferred to the NCF with an undetermined cause of death. He said the body was not identified as a suspected COVID-19 case, they buried it and later learned that it had tested positive.
The CPI also received complaints of the reverse communication problem: family members who are not informed about the test result of their loved one and find out through the funeral home that their loved one had tested positive.
Conte said it is the NCF’s responsibility to report the test results of their cases to the funeral homes, but that it is the Puerto Rico Department of Health’s responsibility to disclose those results and the results of the other tests they handle —including those done by hospitals— to the relatives of the deceased.
This is exactly the basis of the contact tracing strategy that the agency has been trying to implement to identify the people who were potentially exposed to COVID-19 who should be tested, isolated and followed-up on.
On Tuesday, Secretary González said the team working on the issue had already contacted 84% of the people who were in contact with the 915 unique positive cases that the agency had registered.
After experiencing a problem of duplicate and triplicate cases in the reports for COVID-19 tests and results, Puerto Rico’s Health Department revealed a revised number of positives on Tuesday and as of Wednesday it was the last figure available.
Editor’s Note—As of this posting, Puerto Rico’s new dashboard is reporting the following:
This is the latest from #PuertoRico
Now it is saying 1,276 known positive cases. The dashboard now doesn't have how many tests have bee conducted.
77 deaths
That's a 6% death rate, which is big jump from yesterday.
— Julio Ricardo Varela (@julito77) April 24, 2020
Puerto Rico’s Department of Health website is not running:
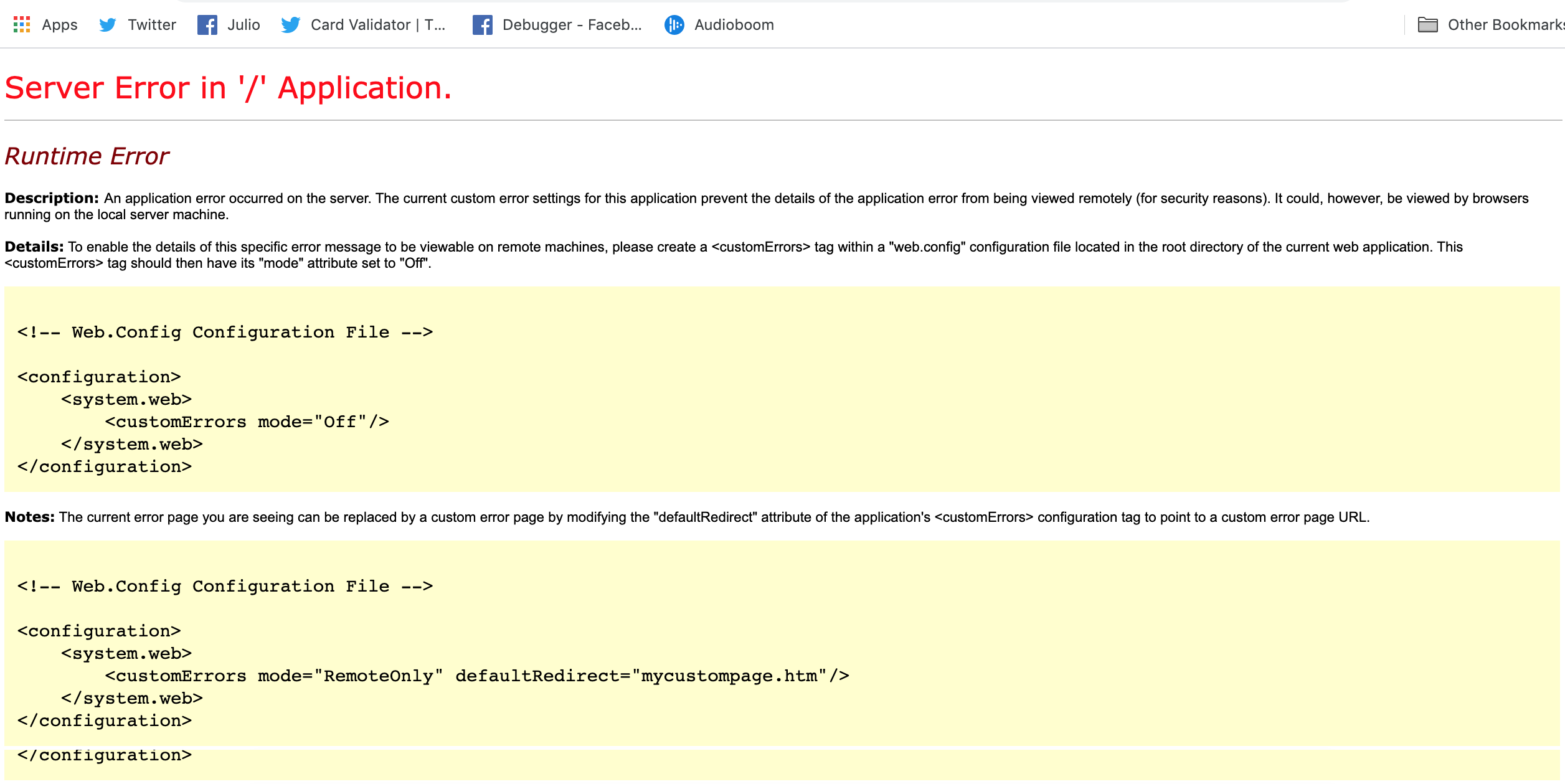
Screen grab, 4:20pm ET Friday, April 24, 2020
***
Eliván Martínez Mercado contributed to this story.